The Intriguing Phenomenon of Ocular Migraines
Read time: 4 minutes
The world of migraines is complex and multifaceted, often bringing with it not only intense headaches but also a spectrum of visual disturbances. Among these, ocular migraines stand as a distinct and intriguing phenomenon. In this blog, we’ll take a deeper look at ocular migraines.
Defining Ocular Migraines
Ocular migraines, also known as retinal, visual, or ophthalmic migraines, are a specific type of migraine that involves visual disturbances or loss of vision in one eye. Unlike traditional migraines that primarily cause headaches, ocular migraines are characterized by temporary visual impairment or changes.
Ocular migraines are considered relatively rare, accounting for a small percentage of all migraine cases. They often occur in individuals who have a history of migraines with or without headaches.
The visual symptoms of ocular migraines typically last less than an hour, and they often precede or accompany a migraine headache. The duration of the visual disturbances is transient, but it can be a cause of concern due to its impact on daily activities.
Characteristics of Ocular Migraines
The hallmark of ocular migraines is the occurrence of visual disturbances in one eye. These disturbances can manifest as:
- Scotomas: Blind spots or areas of reduced vision.
- Flashing Lights: Perceived flashes of light or shimmering zigzag patterns.
- Blindness: Temporary loss of vision in one eye.
Ocular migraines typically affect one eye at a time. The visual disturbances occur on the same side as the subsequent headache if one occurs.
While ocular migraines are often associated with migraines that include headaches, they can occur without any subsequent head pain. This makes the diagnosis and understanding of ocular migraines more challenging.
Causes of Ocular Migraines
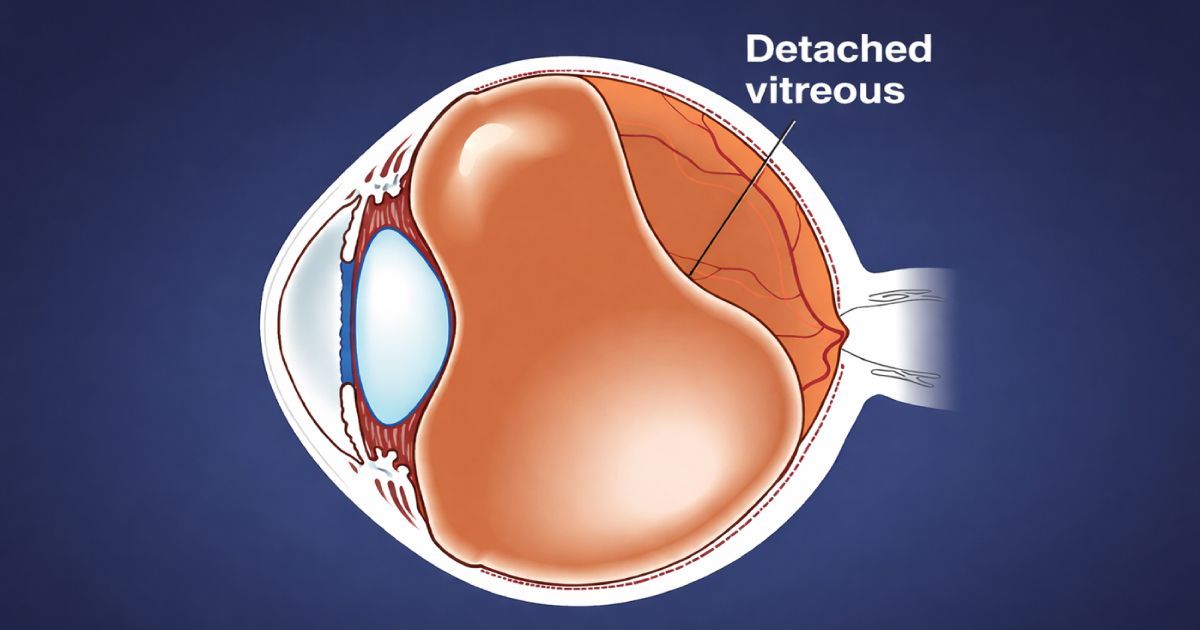
- Vascular Changes: Ocular migraines are believed to be related to temporary changes in blood flow to the visual areas of the brain or the retina. These changes can lead to the visual disturbances characteristic of ocular migraines.
- Spasms of Blood Vessels: The exact cause of the vascular changes is not fully understood, but it is thought to involve spasms or constriction of blood vessels in the eye or brain. This constriction may reduce blood flow temporarily, resulting in visual symptoms.
Ocular Migraine Triggers
Ocular migraines, like traditional migraines, can be triggered by various factors, including:
- Stress and Anxiety
- Certain Foods or Beverages
- Hormonal Changes in Women
- Bright Lights or Flickering Lights
- Dehydration
- Lack of Sleep
- Intense Physical Activity
Symptoms of Ocular Migraines
The primary symptoms of ocular migraines are visual disturbances, which may include:
- Blind spots
- Flashes of light
- Zigzag patterns
- Temporary blindness in one eye
- Headache (Not Always Present): While ocular migraines are not always followed by headaches, some individuals may experience a headache after or during the visual disturbances. The headache may be on the same side as the affected eye.
- Nausea and Vomiting (Rare): In rare cases, individuals may experience nausea and vomiting along with ocular migraines, especially if they progress to a more generalized migraine.
Diagnosis of Ocular Migraines
Diagnosing ocular migraines is like solving a puzzle, and it starts with a detailed checkup by a healthcare expert. They'll ask you lots of questions about when and how often these eye issues happen to figure things out.
The next step is a thorough eye check to make sure there's nothing else causing the problem. They'll also look at how well you can see. Since migraines have to do with your brain, they'll do a careful check on how it's working.
In some cases, they might suggest more detailed tests like an MRI to get a closer look at your brain's structure. Putting all these pieces together helps the experts understand what's going on with ocular migraines.
Treatment Options for Ocular Migraines
- Pain Management (If Headache Occurs): If ocular migraines are followed by headaches, pain management strategies commonly used for migraines may be employed. This may include over-the-counter or prescription medications.
- Lifestyle Modifications: Identifying and avoiding triggers is a key aspect of managing ocular migraines. Lifestyle modifications such as stress management, adequate hydration, regular sleep, and a balanced diet may help reduce the frequency of episodes.
- Prescription Medications: For individuals experiencing frequent or severe ocular migraines, healthcare providers may prescribe medications specifically designed to prevent migraines. These may include beta-blockers, calcium channel blockers, or anti-epileptic drugs.
- Managing Underlying Conditions: If ocular migraines are associated with underlying conditions such as hypertension or hormonal imbalances, managing these conditions may contribute to symptom relief.
Prognosis and Impact on Daily Life
Ocular migraines are generally considered benign, and the visual disturbances are temporary and reversible. Most individuals do not experience any permanent vision loss.
While the visual symptoms of ocular migraines are transient, they can have a significant impact on daily activities, especially if they occur frequently. Driving or operating heavy machinery during an episode is not advisable.
The frequency and severity of ocular migraines vary among individuals. Some may experience occasional episodes with minimal impact, while others may find them more disruptive.
The Takeaway
Ocular migraines present a unique facet of the complex migraine spectrum, characterized by temporary visual disturbances in one eye. Despite their generally benign nature, the transient nature of these disturbances can be alarming and necessitates a thorough evaluation by healthcare professionals. As research continues to unravel the intricacies of migraines, including ocular migraines, a holistic approach to their management and prevention remains crucial for enhancing the quality of life for those affected by this enigmatic phenomenon.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.