Unveiling the Silent Thief: A Guide to Glaucoma
Read time: 7 minutes
Glaucoma, a group of eye conditions that can lead to vision loss and blindness, has been a subject of medical interest and research for centuries. In this guide, we will look into the historical context of glaucoma, explore contemporary insights, and discuss the signs, symptoms, and potential treatment plans.
Glaucoma is the leading cause of irreversible blindness worldwide. In the United States, it is the second leading cause of blindness after macular degeneration. Glaucoma affects over 3 million Americans and 60 million people worldwide. It is a progressive disease that damages the optic nerve, which is responsible for transmitting visual information from the eye to the brain. If left untreated, glaucoma can eventually lead to complete blindness.
The Historical Perspective
The earliest known references to glaucoma can be traced back to ancient Greece, where the term "glaukos" was used to describe a cloudy or green-blue discoloration of the eye. This discoloration was likely a description of the opaque appearance of the eye caused by elevated intraocular pressure (IOP), a key characteristic of glaucoma.
Throughout the centuries, various medical texts and treatises have mentioned glaucoma and its associated symptoms. In the 11th century, the Persian scholar Avicenna provided one of the earliest detailed descriptions of the condition, including its potential to cause blindness. However, it wasn't until the 18th century that significant advancements in understanding glaucoma were made.
In 1756, the German ophthalmologist Georg Joseph Beer introduced the term "glaucoma" to describe the condition characterized by increased intraocular pressure and associated vision loss. Beer's contributions laid the foundation for further research and understanding of this eye disease.
The 19th and early 20th centuries witnessed remarkable progress in the diagnosis and treatment of glaucoma. In 1856, the ophthalmologist Albrecht von Graefe introduced the concept of iridectomy, a surgical procedure that involved removing a portion of the iris to lower intraocular pressure. This procedure, though no longer commonly used, marked a significant milestone in the management of glaucoma.
As scientific knowledge and technological advancements progressed, our understanding of glaucoma deepened. The invention of the ophthalmoscope in the mid-19th century allowed for better visualization of the optic nerve, a crucial element in diagnosing and monitoring glaucoma.
Contemporary Insights
In recent decades, our understanding of glaucoma has grown significantly, thanks to extensive research and advancements in medical technology. We now recognize glaucoma as a diverse group of eye conditions characterized by progressive damage to the optic nerve, often associated with elevated intraocular pressure.
One of the key contemporary insights is the recognition of different types of glaucoma, each with its own characteristics and risk factors. The two main types are:
- Open-angle Glaucoma: This is the most common form of glaucoma, accounting for approximately 90% of cases. In open-angle glaucoma, the drainage angle of the eye remains open, but the trabecular meshwork (the drainage system) becomes less efficient at draining the aqueous humor, leading to increased intraocular pressure. Aqueous humor is the transparent liquid that continuously circulates within the anterior chambers of the eye, performing the vital roles of supplying nutrients to the avascular structures like the cornea and lens while simultaneously generating intraocular pressure, a precisely regulated force that maintains the eye's shape and optical integrity.
- Angle-closure Glaucoma: Also known as narrow-angle or acute glaucoma, this type occurs when the iris obstructs the drainage angle, preventing the proper flow of aqueous humor and resulting in a rapid and dangerous rise in intraocular pressure.
Another significant development is the identification of various risk factors associated with glaucoma. These include age, family history, ethnicity, underlying medical conditions (such as diabetes and hypertension), and certain medications. African Americans are at particularly high risk for the disease. Glaucoma can also be caused by injuries to the eye or certain eye surgeries. Regular eye exams are the best way to catch glaucoma early so that treatment can be started.
Advances in diagnostic techniques have also played a crucial role in improving glaucoma management. Technologies like optical coherence tomography (OCT) and visual field testing have revolutionized the way we detect and monitor optic nerve damage and vision loss associated with glaucoma.
Signs and Symptoms
Glaucoma is often referred to as the "silent thief of sight" because it can progress without noticeable symptoms, especially in the early stages. However, there are certain signs and symptoms that patients should be aware of:
- Gradual Vision Loss: One of the most common symptoms of glaucoma is a gradual loss of peripheral (side) vision. This vision loss can progress slowly and may go unnoticed until significant damage has occurred.
- Tunnel Vision: In advanced stages of glaucoma, the remaining vision may resemble looking through a tunnel, with only a small central area of clear vision remaining.
- Eye Pain and Redness: In acute angle-closure glaucoma, patients may experience severe eye pain, redness, and blurred vision, along with nausea and vomiting. This is considered a medical emergency and requires immediate treatment.
- Halos Around Lights: Some patients with glaucoma may notice halos or rainbow-colored circles around lights, particularly in low-light conditions.
- Frequent Vision Changes: Fluctuations in vision or the need for frequent changes in prescription glasses or contact lenses can be an indicator of glaucoma.
It is important to note that not all individuals with glaucoma experience noticeable symptoms, especially in the early stages. Regular comprehensive eye examinations are essential for early detection and prevention of vision loss.
Treatment Options
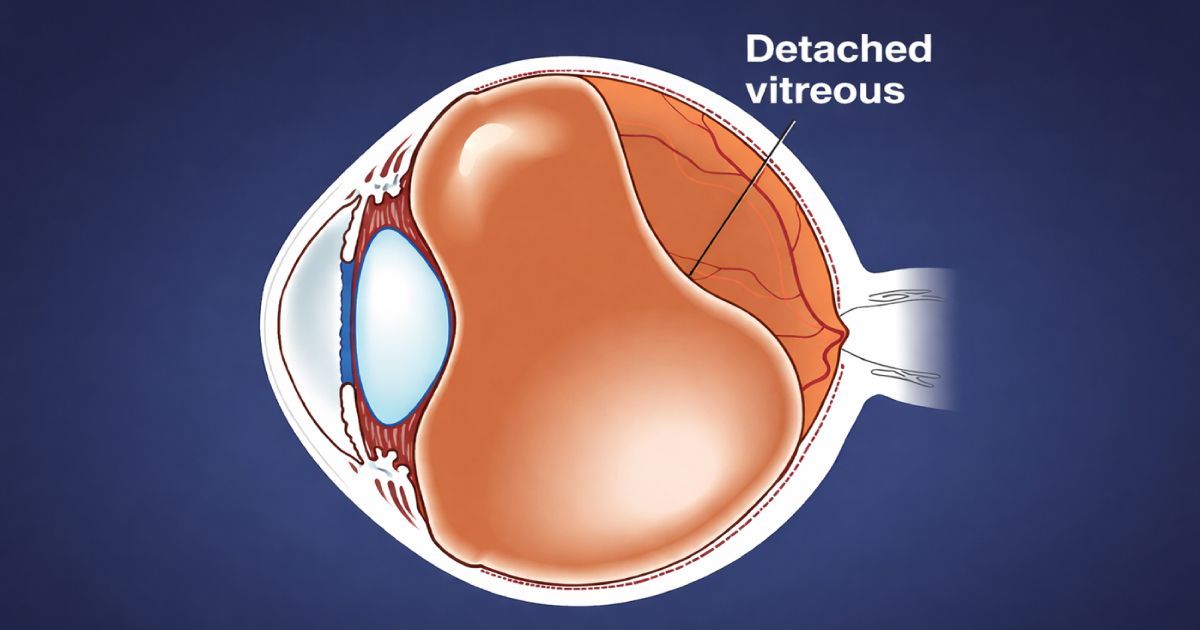
Glaucoma is often linked to an increase in intraocular pressure (IOP). This pressure hike can damage the optic nerve, disrupting the transmission of visual information to the brain. While glaucoma is a progressive condition, various treatment options are available to manage the disease and preserve vision. The goal of treatment is to lower and maintain a safe level of intraocular pressure, preventing further optic nerve damage and vision loss.
- Medications: Eye drops and oral medications are often the first line of treatment for glaucoma. These medications work by either reducing the production of aqueous humor or improving its drainage from the eye, effectively lowering intraocular pressure.
- Laser treatment: Laser procedures, such as selective laser trabeculoplasty (SLT) and argon laser trabeculoplasty (ALT), can be used to improve the drainage of aqueous humor from the eye, thereby reducing intraocular pressure.
- Surgical interventions: In cases where medications or laser treatments are ineffective or unsuitable, surgical procedures may be recommended. These include:
- Trabeculectomy is a procedure that creates a new drainage pathway for aqueous humor to leave the eye.
- Glaucoma Drainage Devices are implantable devices designed to facilitate the drainage of aqueous humor from the eye.
- Minimally Invasive Glaucoma Surgery (MIGS) offers a range of newer, less invasive surgical techniques that aim to improve aqueous humor drainage.
It is important to note that the choice of treatment depends on various factors, including the type and severity of glaucoma, the patient's overall health, and the potential risks and benefits of each option. Regular follow-up appointments and monitoring are crucial to ensure the effectiveness of the chosen treatment plan.
If you have glaucoma, or are at risk for the condition, there are things you can do to help prevent vision loss. These include eating a healthy diet, exercising regularly, and not smoking. You should also avoid using steroids, and wear sunglasses and a hat when you’re outside to protect your eyes from the sun.
The Takeaway
Regular comprehensive eye examinations are crucial for detecting glaucoma in its early stages, when treatment is most effective. If you or a loved one experiences any concerning vision changes or falls into a high-risk category for glaucoma, it is essential to consult with an eye care professional promptly.
Remember, early intervention and adherence to the recommended treatment plan can significantly improve the chances of maintaining good vision and preventing further vision loss. At Urban Optiks Optometry, we are committed to providing our patients with the highest quality of care and personalized treatment plans tailored to their individual needs.
Share this blog post on social or with a friend:
The information provided in this article is intended for general knowledge and educational purposes only and should not be construed as medical advice. It is strongly recommended to consult with an eye care professional for personalized recommendations and guidance regarding your individual needs and eye health concerns.
All of Urban Optiks Optometry's blog posts and articles contain information carefully curated from openly sourced materials available in the public domain. We strive to ensure the accuracy and relevance of the information provided. For a comprehensive understanding of our practices and to read our full disclosure statement, please click here.